Introduction
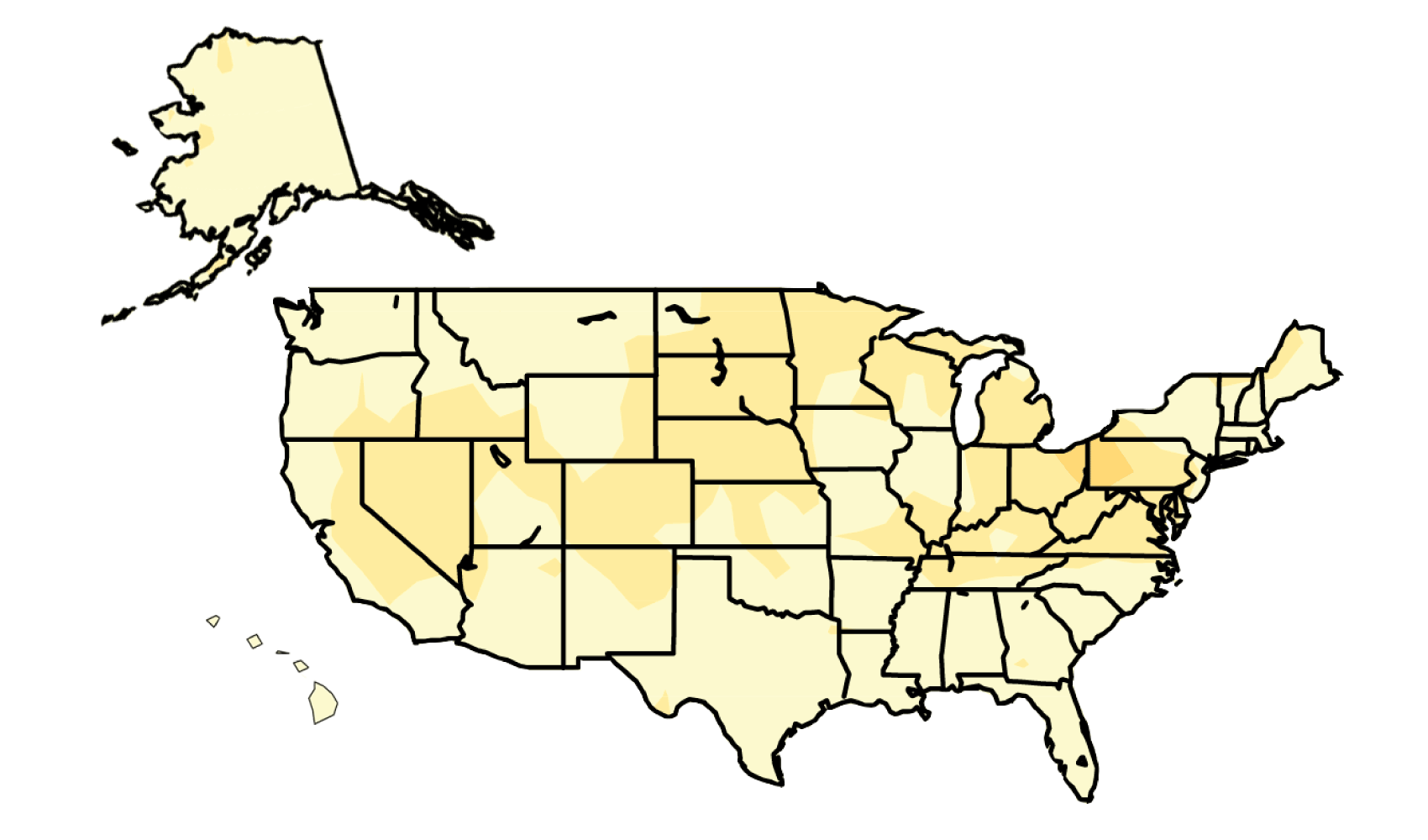
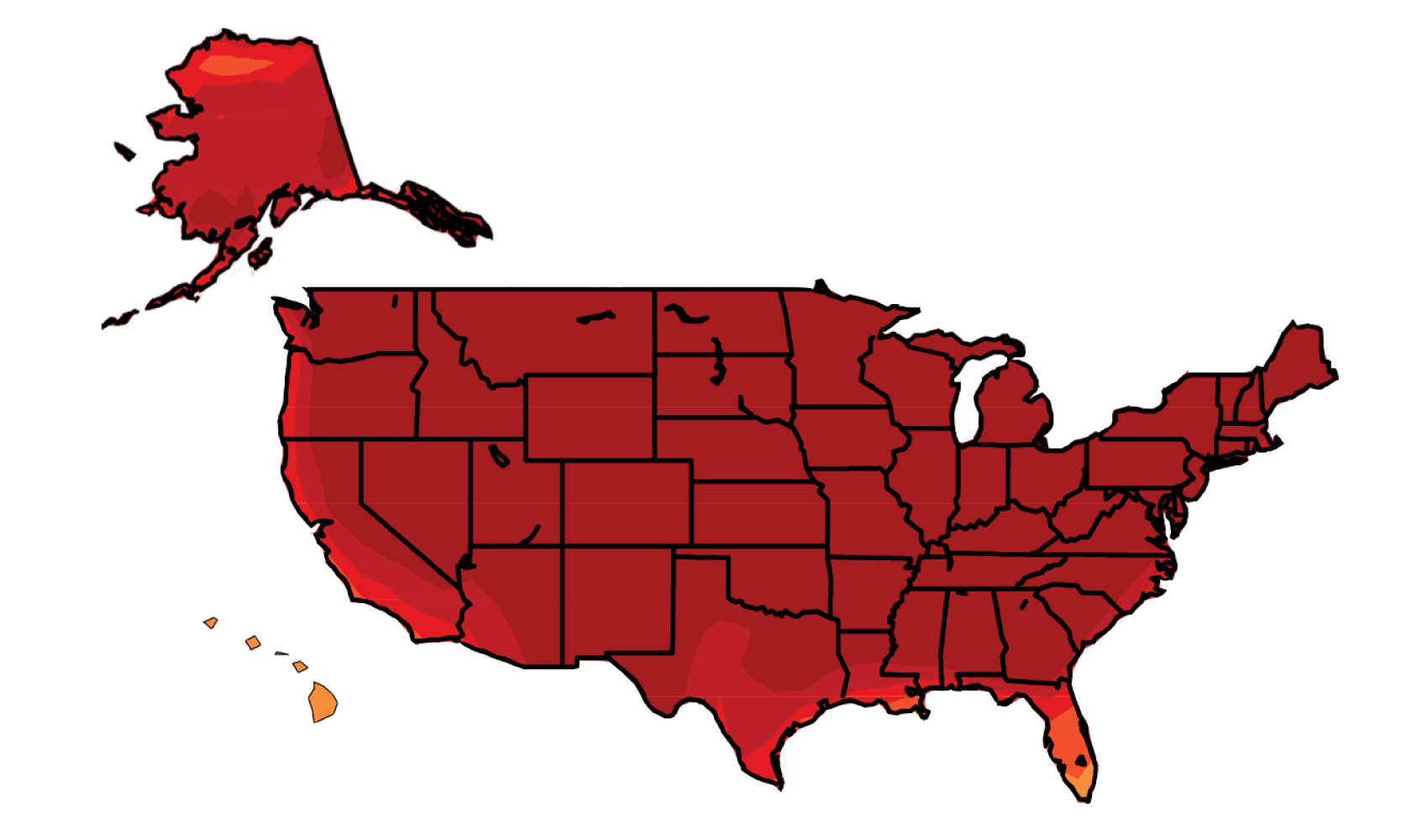
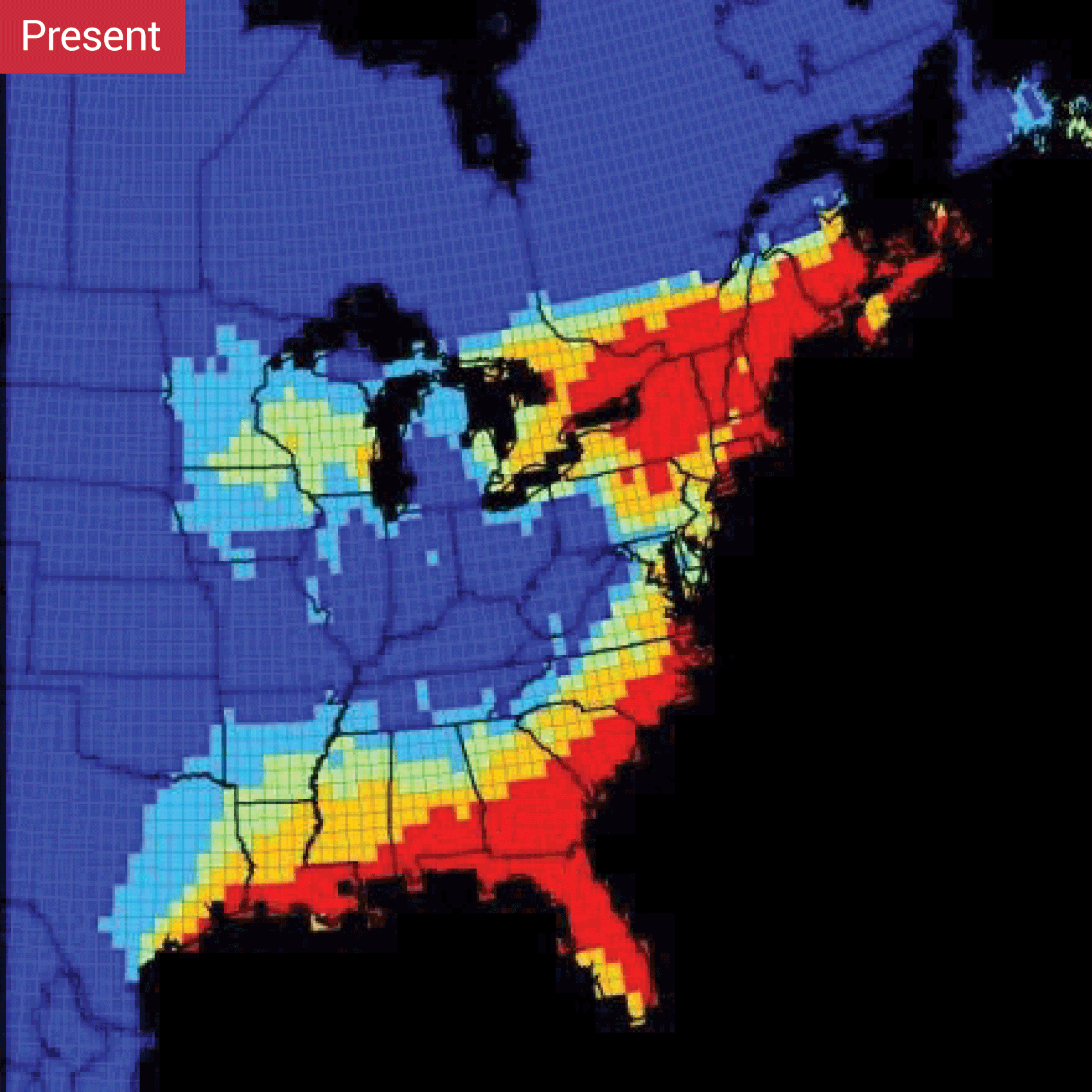
Climate change is increasing the risks of respiratory stress from poor air quality, heat stress, and the spread of food-borne, insect-borne, and waterborne diseases. Extreme weather events often lead to fatalities and a variety of health impacts on vulnerable populations, including impacts on mental health, such as anxiety and post-traumatic stress disorder. Large-scale changes in the environment due to climate change and extreme weather events are increasing the risk of the emergence or reemergence of health threats that are currently uncommon in the United States, such as dengue fever.
Key weather and climate drivers of health impacts include increasingly frequent, intense, and longer-lasting extreme heat, which worsens drought, wildfire, and air pollution risks; increasingly frequent extreme precipitation, intense storms, and changes in precipitation patterns that can lead to flooding, drought, and ecosystem changes; and rising sea levels that intensify coastal flooding and storm surge, causing injuries, deaths, stress due to evacuations, and water quality impacts, among other effects on public health.